
An ulcer is a breach in the continuity of skin, or mucous membranes; dead tissue sloughs away, leaving a raw, painful tissue bed. Ulcers can occur right along the gastrointestinal tract, but are most often in the mouth (usually due to dental disease), and the stomach. The horse’s stomach is split into two distinct sections – the upper squamous mucosa and the lower glandular mucosa.
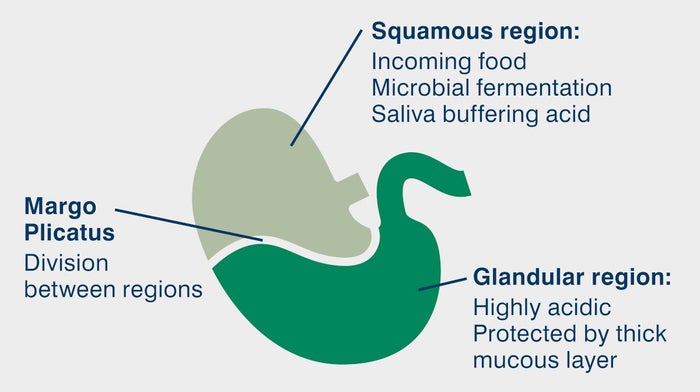
The squamous part of the stomach expands slightly to hold food, but otherwise is almost non-functional. It does not produce stomach acid, and is poorly protected against it compared to the glandular portion. In the wild, horses will eat for up to 18 hours per day. This constant chewing and swallowing produces saliva which enters the stomach, coats the squamous mucosa and helps to buffer or neutralise the gastric acid. The coarse grass and forage that the horse has evolved to eat produces a ‘fibre matt’ in the stomach which again helps to prevent stomach acid from damaging the squamous mucosa.
Unfortunately, modern practices such as stabling, feeding large meals at either end of the day, and replacing forage with high starch concentrate feeds, reduce these natural protective effects. It is this that underpins the development of squamous ulcers.
The glandular part of the stomach produces the stomach acid, and consequently has a thick protective mucous coating. It is much more resilient to the caustic stomach acid, but can still be affected by ulceration. Again, ulceration has been linked to feeding and management practices, but in the glandular region an underlying impairment in mucous production or reduced blood flow to the stomach lining is also implicated.
Top tip: The squamous lining resembles that of the oesophagus and when acid comes into contact with this mucosa it could be compared to acid reflux or heart burn in people which is distinctly painful.
Risk Factors
Discontinuous/intermittent feeding and starving - The horse’s stomach constantly produces gastric acid so every minute a horse is without food, and therefore is not producing saliva, the stomach becomes more acidic, putting the stomach lining at risk. A horse left without forage for over 6 hours overnight is 4 times more likely to develop glandular ulcers.
Exercise – especially fast exercise or jumping. During exercise the stomach acid splashes onto the upper squamous mucosa. This is especially so if the horse has been starved prior to exercise – a common management practice.
Feeding starch – starch encourages the growth of health negative bacteria in the stomach, which ferment the starch and produce lactic acid. Studies have shown that feeding over 2g per kg body weight of starch per day increases the risk of ulceration.
Stress – stressed horses eat less, and stress related hormonal changes can directly compromise the stomach lining.
Stereotypes – repetitive behaviour such as crib biting and wind sucking is associated with ulcers. It is not known if they are a cause of ulcers – more time crib biting means less time eating – or an effect of having ulcers – the horse is trying to ease the pain in the stomach.
Anti-inflammatory use – use of non-steroidal anti-inflammatory drugs at above the recommended dose has been linked to the development of glandular ulcers, as they interfere with mucous production.
Top tip: Anti-inflammatories such as Phenylbutazone and Flunixin are only thought to be a problem when given at high doses or for long periods.
Are ulcers common?
In a word: yes! In some studies squamous ulcers have been found in close to 100% of race and endurance horses in training, and 40-60% of pleasure and show horses. Glandular ulcers have recently been found in 54% of pleasure horses and 64% of sports horses in the UK. The difference in incidence between groups is due to the different stress levels and management practices involved – centred on stabling, feed and exercise.
Clinical Signs and Diagnosis
The clinical signs of gastric ulceration can be vague and varied. Some horses may accept the pain in their stomach and show no signs at all, many will have a reduced appetite, behavioural changes (such as grumpiness, and resentment of girthing or riding), and poor performance, with some progressing to weight loss and colic. Diagnosis must be made by gastroscopy. Passing a camera into the stomach of a starved horse and visualising the stomach lining is the only way to accurately diagnose and grade ulcers.
Other tests such as faecal blood tests cannot differentiate between blood from ulceration or from a variety of other causes such as worms.
Treatment
If their horse is diagnosed with gastric ulcers many owners will think first of pharmaceutical treatment. For squamous ulceration, omeprazole treatment is very successful, as it blocks the pumps which produce the stomach acid. Roughly 80% of horses with ESGD are healed within 28 days of omeprazole therapy. For glandular ulcers the success rate drops to 25% after 28 days of therapy. This is thought to be because of the more complex underlying causes involved in EGGD. Omeprazole treatment should be extended and other drugs can be added to the treatment regimen to protect the mucosa or to boost mucous production. However, for the successful treatment of both conditions, long term management changes are vital to remove the underlying risk factors.
Despite some conflicting reports, continuous turn out is considered to be the best management practice for horses with ulcers. Failing this, forage should be fed ad lib, or frequently throughout the day – avoiding a gap of six hours or more. Little or no hard feed should be given, and the total starch content of the diet should be less than 2g per kg body weight per day. Feeding oil such as corn oil has been shown to reduce gastric acid output and slow gastric emptying. Exercise and transport have both been implicated in ulcer development and so should be minimised. Starving before exercise is not advised; indeed feeding a small handful of chaff before riding may help to soak up the gastric acid, and reduce splashing on the stomach wall.
Gastric ulceration is a common and debilitating condition largely caused by our domestication and management practices. Whilst prevention and treatment must centre on management change, effective options are available to reduce acidity and soothe the gut lining.
Omeprazole blocks the body’s communication with the acid pumps and keeps them switched off. When they stop producing acid the body asks them to produce more but the signals can’t get through. However, when the omeprazole treatment ends, suddenly this build-up of signals can produce a large release of acid which can cause further ulceration! Speak to your vet about tapering down omeprazole treatment before ending it.









